Diabetic Retinopathy
Diabetic retinopathy is an eye condition that affects people who have had diabetes for some years. However, as current statistics show that about half of the diabetics in Canada are, as yet, undiagnosed, the incidence is probably more prevalent than the statistics show. Certainly, the number of cases of diabetic retinopathy is increasing significantly.
According to the World Health Organization, the incidence of diabetes is rising at an alarming rate. During this decade alone, the number of diabetics will increase by almost 25%, rising from 177 million cases worldwide in 2000 to 221 million cases by 2010. By 2030, it is estimated that the number will have reached 370 million.
In Canada, the growth rate is even more dramatic, with an anticipation that this decade will see the combined diagnosed and undiagnosed diabetics increasing from 1 million to 3 million people.
Significantly, this is also the eye problem that generally affects the younger — working — generation. While many of the other retinal diseases are associated with people over the age of 60, diabetic retinopathy is seen among people from late teens to mid 50s.
Two Alternative Diagnoses
There are two forms of this condition - background retinopathy and the more serious proliferative retinopathy. Essentially, both are caused by poorly controlled blood sugar levels, which damage the blood vessels in the retina.
Vision is not normally affected with background retinopathy. When vision is affected it is the result of macular edema and/or macular ischemia. Macular edema, the most common cause of loss of vision in diabetes, is a result of the swelling, or thickening of the macula, the central part of the retina that enables people to see fine details. Macular ischemia, in turn, is the result of the closure of blood vessels supplying the macula.
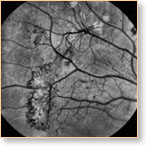
Proliferative retinopathy is the result of new, fragile blood vessels growing over the surface of the retina. Their fragility usually leads to them breaking and bleeding into the vitreous in the eye. This clouds the vision, and although the impairment may disappear, it usually returns with increasing effect, with the potential of leading to blindness.
Patients with diabetic retinopathy visiting Dr. Uniat will initially have their pupils dilated, to have their retinas more effectively visualized through special lenses and the ophthalmoscope or microscope. A detailed analysis of the extent of damage will then be carried out — either with the Centre's OCT (optical coherence tomography) unit or fluorescein angiography at the Royal Alexandra Hospital.
Treatment
Little, if any, treatment is required for background retinopathy, other than controlling one's diet.
If the condition is more serious and is threatening vision, it is likely that Dr. Uniat will provide laser treatment in her clinic. The laser beams can stop discrete retinal leakages. They can also create hundreds of tiny burns to prevent swelling and congestion of the abnormally proliferating blood vessels.
In severe cases, where the abnormal blood vessels and blood seepage are too dense for laser beam penetration, a hospital surgery called vitrectomy is required. During vitrectomy, delicate instruments are used inside the eye to remove the vitreous gel, or intraocular hemorrhage that may occur with diabetic retinopathy. Dr. Uniat performs this surgery — under local or general anesthetic — at the adjacent Royal Alexandra Hospital. This particular surgery has a risk of complications and is used only with the most advanced cases of diabetic retinopathy that are otherwise untreatable.